An experienced medical marijuana doctor in Naples can potentially help some patients manage anxiety or PTSD symptoms by certifying access to medical cannabis and guiding individualized treatment plans based on the endocannabinoid system. This article explains what that pathway looks like, how cannabis compounds like THC and CBD interact with CB1/CB2 receptors, and what current research and clinical experience indicate about benefits and risks for anxiety and PTSD. Many readers want clear, practical steps: who qualifies in Florida, how clinicians assess suitability, what products and delivery methods are commonly used, and how to reduce risk while tracking outcomes. The sections below cover mechanisms and evidence, Florida qualification and registration steps, the clinical consultation process, comparative treatment options with an EAV-style product table, safety and side-effect management with a dedicated risk table, and where to look for qualified clinicians in Naples. Throughout the guide you will find plain-language lists, comparison tables, and actionable advice to support an informed discussion with your healthcare team about medical cannabis for mental health.
How Does Medical Marijuana Treat Anxiety and PTSD in Naples?
Medical marijuana treats anxiety and PTSD primarily by modulating the endocannabinoid system, where cannabinoids interact with CB1 and CB2 receptors to influence stress, fear memory, and arousal pathways. Low-to-moderate doses of THC can produce acute anxiolytic effects in some patients by dampening amygdala hyperactivity, while CBD has been shown to reduce anxiety-related responses through serotonergic and endocannabinoid-mediated mechanisms. Current research indicates symptomatic benefit for sleep disturbance, hyperarousal, and nightmare frequency in some PTSD patients, but evidence quality varies and randomized trial data remain limited. Clinically, cannabis is often used as part of a broader treatment plan that includes psychotherapy and, when appropriate, pharmacotherapy; it is best considered a symptomatic option rather than a definitive cure. Understanding mechanisms and evidence helps patients set realistic expectations and fosters a collaborative treatment plan with their Naples clinician.
Further research highlights the critical role of the endocannabinoid system in modulating fear and anxiety, suggesting therapeutic avenues for conditions like PTSD.
Endocannabinoid System & PTSD: Modulating Fear & Anxiety with Cannabinoids
Recent discoveries position the endocannabinoid system as a pivotal regulator of fear acquisition, consolidation, and extinction. Clinical observations of altered anandamide levels and cannabinoid receptor CB₁ upregulation in individuals with severe PTSD underscore the therapeutic potential of restoring endocannabinoid tone. Preclinical studies demonstrate that direct CB₁ agonists, fatty acid amide hydrolase (FAAH) inhibitors, and phytocannabinoids such as tetrahydrocannabinol (THC) and cannabidiol (CBD) can facilitate extinction learning and attenuate anxiety-like behaviours.
The Endocannabinoid System in PTSD: Molecular Targets for Modulating Fear and Anxiety, 2025
What Are the Benefits of Medical Marijuana for Anxiety and PTSD?
Medical marijuana can offer symptom relief across several domains that matter for anxiety and PTSD, including reduced acute anxiety episodes, improved sleep, and decreased nightmare frequency, which together can enhance daily functioning. Clinical and patient-reported data suggest benefits for sleep continuity and reductions in intrusive memories or hypervigilance for some individuals, but study heterogeneity and small sample sizes limit broad generalization. Benefits depend on cannabinoid profile, dose, and delivery method; CBD-dominant or balanced THC:CBD formulations often show fewer adverse mood effects than high-THC products. Patients who experience symptom relief typically report improved sleep quality and reduced nighttime hyperarousal, which can make other therapies more effective. These potential benefits should be weighed against limitations of the evidence and individualized through careful clinical follow-up.
While medical cannabis shows promise for symptom relief, a broader systematic review of its efficacy and safety for mental disorders underscores the need for more robust clinical trials.
Efficacy & Safety of Medical Cannabis for Mental Disorders
THC- and CBD-based medicines, given as adjunct to pharmaco- and psychotherapy, were associated with improvements of several symptoms of mental disorders, but not with remission. Side effects occurred, but severe adverse effects were mentioned in single cases only. In order to provide reliable treatment recommendations, more and larger RCTs with follow-up assessments, consistent outcome measures and active comparisons are needed.
How effective and safe is medical cannabis as a treatment of mental disorders? A systematic review, 2019
Common domains where medical cannabis for PTSD may help anxiety and PTSD symptoms:
- Sleep improvement and reduced nightmares, improving daytime functioning.
- Short-term reduction in acute anxiety or panic episodes with controlled dosing.
- Decreased hyperarousal and reactivity in certain PTSD presentations.
These benefits are meaningful for many patients but require careful monitoring and integration with psychotherapy to optimize long-term outcomes.
How Does Cannabis Affect Mental Health Conditions?
Cannabis affects mental health in dose– and compound-dependent ways: low-dose THC or CBD can reduce anxiety for some people, whereas high-dose THC may provoke anxiety, panic, or worsening mood in susceptible individuals. CBD generally shows anxiolytic properties in preclinical and early clinical studies and may counterbalance some THC-related adverse effects, while THC primarily acts on CB1 receptors in the brain to alter fear and reward circuitry. Long-term or heavy use, especially of high-THC products, is associated with increased risk of dependency and cognitive change in vulnerable populations, and there is a small but important psychosis risk in those with predisposition. Clinicians assess these trade-offs when recommending product profiles and dosing strategies, emphasizing lower THC, higher CBD, and careful titration for patients with anxiety or PTSD. Understanding these differential effects helps patients and clinicians select safer, more targeted approaches.
Who Qualifies for a Medical Marijuana Card in Naples for Mental Health?
In Florida, qualification for medical marijuana requires documentation of a qualifying medical condition and clinician certification to register the patient in the state program overseen by the Florida Department of Health’s Office of Medical Marijuana Use. PTSD is recognized as a qualifying condition in Florida’s medical cannabis program, while anxiety-related disorders are not explicitly listed as qualifying conditions but may be considered when documented as a component of a qualifying diagnosis or when accompanied by other qualifying conditions; clinicians document symptoms, prior treatments, and rationale for cannabis use. A qualifying clinician evaluates medical records, psychiatric history, and treatment response before issuing a recommendation; after certification patients register with the state registry to receive an identification card. Patients should prepare supporting documentation such as psychiatric notes, prior medication trials, and records of therapy to streamline evaluation and ensure clear evidence of persistent, treatment-resistant symptoms when applicable. Knowing documentation expectations and registry steps helps patients in Naples approach certification with realistic timelines and required materials.
Florida’s progressive stance on medical marijuana has opened doors for many patients, though navigating the policy and its associated barriers remains a key consideration.
Florida Medical Marijuana Policy: Access & Conditions
Florida became the first state in the U.S. South to legalize the use of medical marijuana to treat a variety of health conditions including chronic pain, epilepsy, and spasticity symptoms from multiple sclerosis. While there are over 200,000 medical marijuana patients in Florida, there remain financial, psychological, and insurance coverage barriers which reduce access for many patients.
Medical marijuana policy reform reaches Florida: a scoping review, K Howell, 2019
| Condition or Document | Requirement | How to document |
| Post-traumatic stress disorder (PTSD) | Clinical diagnosis by a qualified provider | Psychiatric evaluation notes or psychologist/psychiatrist documentation showing DSM-based diagnosis |
| Generalized anxiety or panic disorder (when applicable) | Not a standalone qualifying condition in Florida; may be considered with comorbid qualifying conditions | Clinic notes, medication trials, and therapy records supporting symptom persistence |
| Medical records and treatment history | Evidence of prior therapies and current treatment plan | Copies of relevant medical/psychiatric notes, medication lists, and therapy summaries |
What Are Florida’s Medical Marijuana Qualifying Conditions for Anxiety and PTSD?
Florida’s program centers on clinician-documented qualifying conditions and a state registry process; PTSD is explicitly recognized as a qualifying condition, while primary anxiety disorders are not included on the official list and generally do not qualify unless accompanied by other qualifying diagnoses. Clinicians in Naples will review psychiatric assessments, prior medication trials (such as antidepressants or anxiolytics), and therapy engagement to justify a recommendation when anxiety-related symptoms significantly impair function and are part of a qualifying condition. Documentation that clarifies symptom severity, functional impact, and response to conventional treatments strengthens an application; psychiatric notes, psychotherapy summaries, and medication history are common supporting items. Because state program requirements focus on clinician judgment and documentation, clear medical records and a thoughtful narrative from the treating clinician make qualification more straightforward. Patients should prepare comprehensive records to enable a timely and well-supported certification decision.
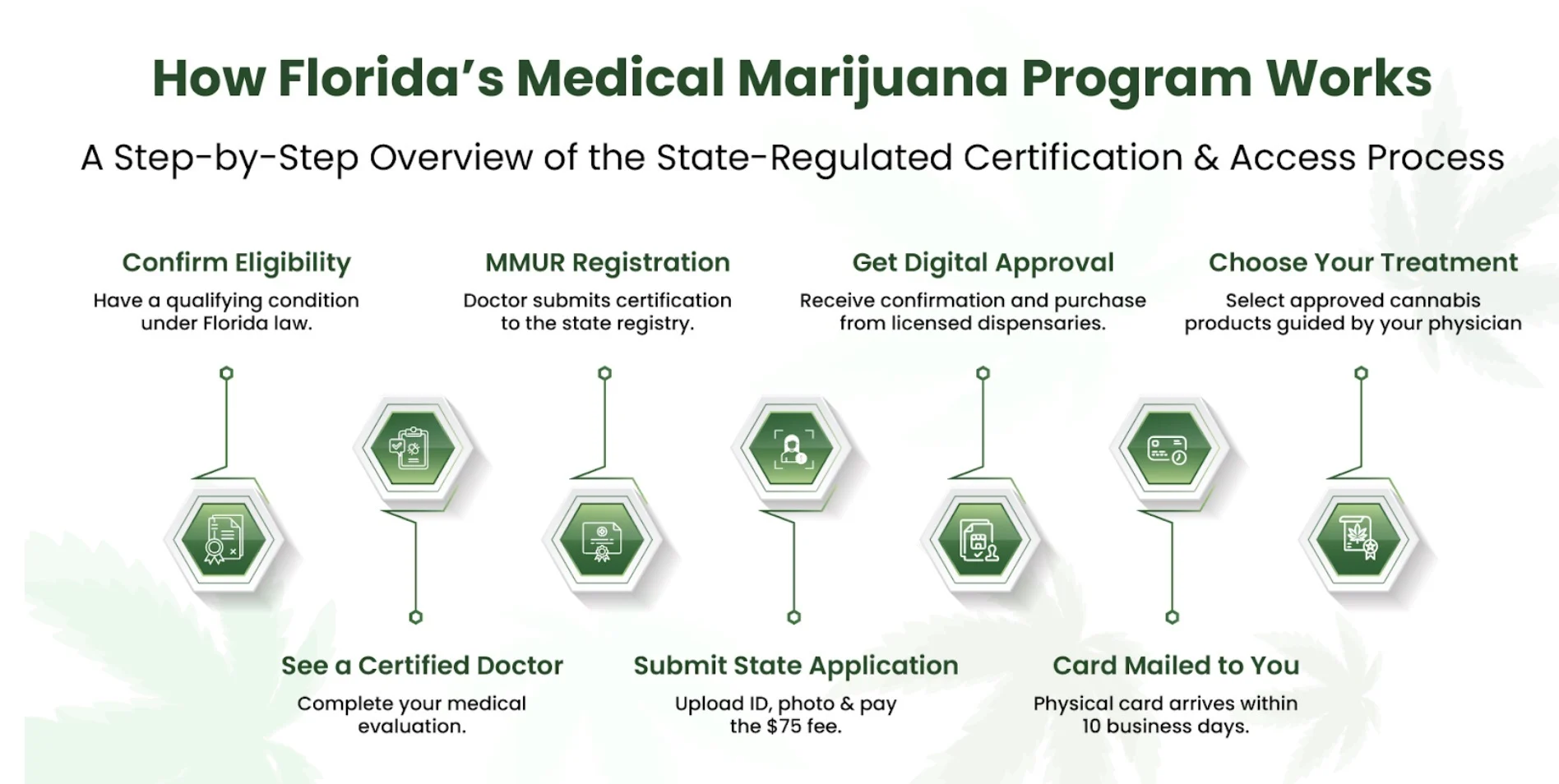
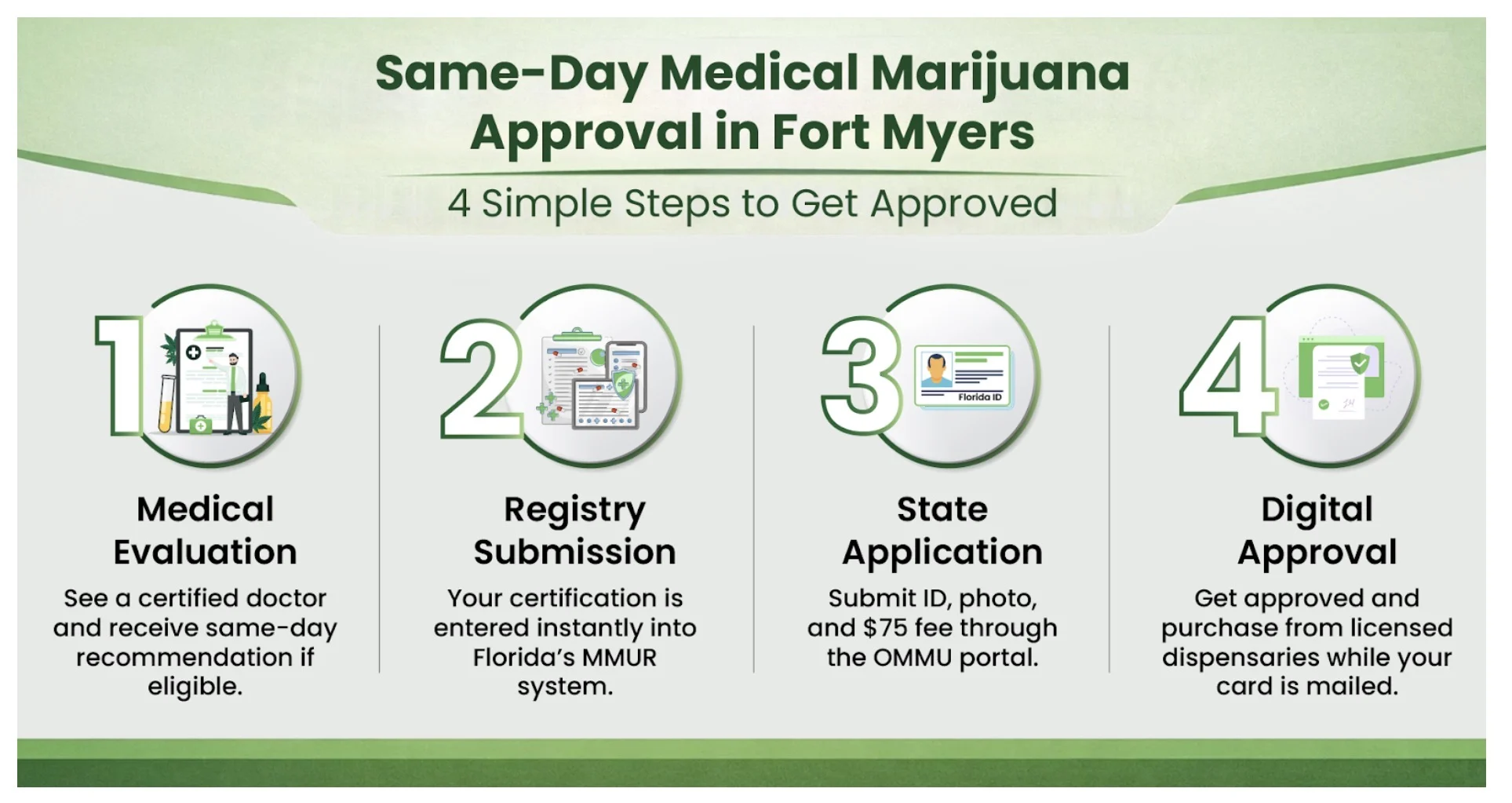
How to Get a Medical Cannabis Card in Naples: Step-by-Step Guide
The process to obtain a medical cannabis card in Naples involves a small number of sequential steps that begin with preparation of medical documentation and end with registry activation after clinician certification. First, gather relevant medical and psychiatric records that document diagnosis, symptom severity, and prior treatments; having clear notes from mental health providers speeds evaluation. Second, schedule and attend a certified clinician evaluation where the clinician reviews records, assesses suitability, and documents a recommendation if appropriate. Third, the clinician submits the required certification to the state medical marijuana registry and the patient completes registration steps to receive an identification card that authorizes legal purchase and use. Typical timelines vary, but preparing records in advance and following up promptly with registry steps can shorten processing time.
- Prepare medical records: Collect psychiatric evaluations, medication lists, and therapy notes.
- Attend clinician evaluation: Meet a certified physician for assessment and recommendation.
- Register with state program: Complete registry steps after clinician certification to receive a card.
These steps provide a clear roadmap for Naples patients seeking legal access to medical cannabis, emphasizing documentation and clinician collaboration.
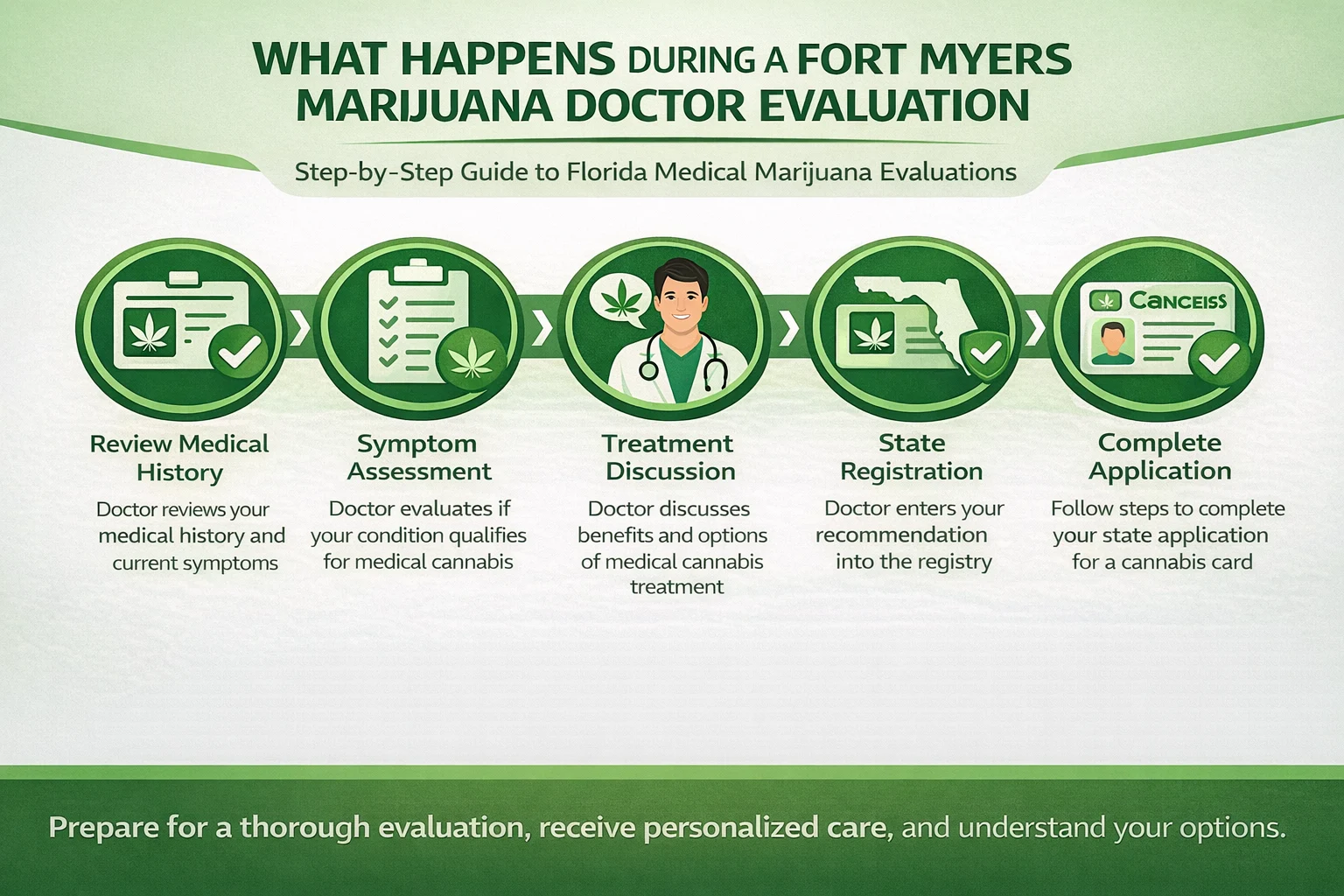
What Should You Expect During a Consultation with a Naples Medical Marijuana Doctor?
A consultation with a Naples medical marijuana doctor typically begins with a focused medical and psychiatric history, medication review, and discussion of treatment goals to determine whether cannabis is appropriate for anxiety or PTSD symptoms. Clinicians use standardized screening tools and clinical interviews to assess severity, comorbidities, substance use history, and suicide risk; this evaluation helps identify contraindications and guides product selection. Expect the clinician to discuss dosing strategies, product profiles (THC vs CBD balance), potential interactions with current psychiatric medications, and a follow-up plan to monitor outcomes and adverse effects. The visit concludes with documentation for the state registry if the clinician recommends medical cannabis, and clear scheduling of follow-up visits to titrate dose and reassess efficacy and safety. Understanding this workflow helps patients arrive prepared and engage effectively in shared decision-making.
How Do Doctors Assess Anxiety and PTSD for Cannabis Treatment?
Doctors assess anxiety and PTSD using a combination of standardized instruments, clinical interviewing, and review of prior treatments to determine appropriateness and risk for cannabis-based therapy. Common screening tools include brief severity measures that quantify symptom burden, while targeted questions evaluate trauma history, functional impairment, comorbid mood disorders, and substance use, all of which influence clinical candidacy. Clinicians specifically screen for psychosis risk, heavy substance use, and unstable medical conditions that may contraindicate cannabis or necessitate alternative strategies. This comprehensive assessment informs whether to recommend CBD-dominant products, low-dose THC regimens, or to advise against cannabis and prioritize other evidence-based therapies. Accurate assessment ensures treatment choices align with patient safety and therapeutic goals.
What Questions Will the Doctor Ask About Your Mental Health?
During the visit, clinicians ask focused questions about symptom onset, frequency, triggers, and prior responses to medications and therapy to build a clear clinical picture and identify treatment goals. Expect questions about sleep patterns and nightmares, functional impairment at work or home, history of trauma, prior psychiatric hospitalizations, and any history of substance misuse or psychotic symptoms. The clinician will also inquire about current medications, over-the-counter substances, and any allergies or medical conditions that could interact with cannabis. Providing candid, detailed answers and bringing concise records of prior treatments helps the clinician recommend the safest and most targeted product and dosing strategy.
- Key items to prepare before the consultation:A concise list of current medications and supplements with doses.Recent psychiatric or therapy notes that document diagnosis and treatment history.Clear descriptions of symptom patterns, triggers, and daily functional impact.
Preparing these items improves the efficiency of the consultation and supports a tailored treatment plan.
What Are the Different Cannabis Treatment Options for Anxiety and PTSD in Naples?
Treatment options for anxiety and PTSD include a range of cannabinoid profiles and delivery methods that vary by THC:CBD ratio, onset, and duration; clinicians personalize choices based on symptom targets like acute panic, chronic hyperarousal, or sleep disruption. Lower-THC, higher-CBD tinctures and balanced formulations are commonly preferred for daytime anxiety management to minimize psychoactive effects, while rapid-onset inhaled options may be used selectively for acute panic or breakthrough symptoms under medical guidance. Longer-acting oral products can support sleep but require careful dosing and patience during titration to avoid next-day sedation; transdermal or topical options have a more limited role for systemic anxiety symptoms. Selecting the right option depends on symptom timing, prior response, comorbidities, and interaction risk, and clinicians typically start with conservative dosing and structured follow-up to adjust therapy.
| Treatment Option | Key Attributes (THC:CBD / Delivery / Onset / Duration) | Recommended Use Case |
| CBD-dominant tincture | Low THC : High CBD, sublingual, onset 20–60 min, duration 4–8 hrs | Daytime anxiety control without intoxication |
| Balanced THC:CBD vape | Moderate THC:CBD, inhaled, onset minutes, duration 2–4 hrs | Acute panic or breakthrough anxiety under supervision |
| Low-dose THC edible | Low THC with measured dosing, oral, onset 1–2 hrs, duration 6–8+ hrs | Sleep disturbances and nightmare reduction when titrated carefully |
| Transdermal patch | Variable THC:CBD, skin delivery, onset hours, duration extended | Steady symptom control with lower peak psychoactive effects |
Which Cannabis Strains Are Recommended for Anxiety and PTSD?
Rather than focusing on strain names, clinicians emphasize chemotype characteristics—cannabinoid ratios and terpene profiles—that influence anxiolytic versus anxiogenic potential, favoring low-to-moderate THC and higher CBD with calming terpenes. Terpenes such as linalool and myrcene are associated with sedative or calming properties, while limonene or pinene may have more stimulating effects; matching terpene balance to symptom needs can refine selection. High-THC strains are generally avoided for patients with significant anxiety or psychosis risk, and clinicians often recommend starting with CBD-dominant or balanced products and titrating slowly. Practical starting ratios often emphasize CBD prominence or 1:1 THC:CBD approaches with careful monitoring of mood and cognition. This chemotype-focused strategy reduces reliance on broad “indica/sativa” labels and enhances predictability of clinical effects.
What Are the Methods of Medical Marijuana Consumption?
Consumption methods vary in onset, duration, and dose control, offering options to match symptom timing—rapid-onset inhalation for acute panic, sublingual tinctures for measured dosing, or oral products for overnight sleep support. Inhalation provides minutes-to-peak effects and shorter duration, useful for sudden severe anxiety but carries respiratory considerations; sublingual tinctures offer more controlled absorption with intermediate onset and duration. Edibles provide long-lasting coverage but require slow titration due to delayed onset and variable metabolism, making them better suited for nighttime symptoms like nightmares. Topicals and transdermals have softer systemic profiles and are less commonly used for core anxiety symptoms but may suit patients seeking low systemic exposure. Choosing a method requires balancing rapid relief needs against safety and predictability.
Methods summary:
- Inhalation (vaping/smoking): Fast onset, short duration, useful for acute symptoms but with respiratory considerations.
- Sublingual tinctures: Moderate onset and duration with more precise dosing control.
- Oral edibles/capsules: Slow onset, long duration, helpful for sleep but require careful titration.
Are There Risks or Side Effects of Using Medical Marijuana for Anxiety and PTSD?
Medical cannabis carries several potential risks including short-term adverse effects, interaction with psychiatric medications, dependence risk, and a modest increased risk of psychosis in predisposed individuals; clinicians assess and mitigate these before and during treatment. Short-term side effects commonly include drowsiness, dry mouth, dizziness, and cognitive slowing, which can impair driving or workplace performance. Drug interactions—particularly with sedating psychiatric medications, benzodiazepines, or medications metabolized by the same liver enzymes—require clinician review and sometimes dose adjustments. Long-term heavy use is linked to dependence and cognitive changes in certain populations, so clinicians recommend the lowest effective dose, regular monitoring, and coordination with mental health providers to detect early signs of adverse outcomes.
| Side Effect / Risk | Likelihood | Mitigation Strategy |
| Drowsiness / sedation | Common | Use lower doses, avoid driving until response known |
| Increased anxiety or panic (high-THC) | Possible in susceptible individuals | Prefer low-THC or CBD-dominant products and slow titration |
| Cognitive slowing / memory effects | Possible with chronic high-dose THC | Limit THC exposure and monitor cognitive function over time |
| Dependence / withdrawal | Uncommon to moderate with long-term use | Use treatment contracts, regular follow-up, and tapering plans if needed |
What Are Common Side Effects Patients Should Know?
Patients commonly experience mild-to-moderate side effects such as sleepiness, dry mouth, lightheadedness, and short-term memory lapses, which are usually dose-related and reversible with dose adjustment. High doses of THC can cause acute anxiety, paranoia, or panic in susceptible individuals, so starting with low THC and gradually increasing under clinician supervision reduces this risk. If side effects are persistent, severe, or include suicidal ideation, psychosis, or loss of consciousness, patients should stop the product and seek immediate medical evaluation. Communicating side effects to the prescribing clinician allows safe titration and alternative strategies, such as switching to CBD-dominant formulations or non-cannabinoid therapies. Proactive monitoring and education minimize harm while preserving therapeutic benefit.
How to Use Medical Marijuana Safely for Mental Health Conditions?
Safe use follows the “start low, go slow” principle with clear documentation, symptom tracking, and regular clinician follow-up to assess efficacy and adverse effects over time. Patients should maintain a symptom diary noting dose, product type, timing, and symptom response to guide titration and identify patterns, and they should avoid combining cannabis with alcohol or sedative medications without clinician approval. Coordinate care with mental health providers and inform all prescribers about cannabis use to prevent interactions and ensure integrated treatment. Finally, use conservative THC exposure, favor CBD or balanced products when appropriate, and schedule periodic reassessments to consider dose reduction or discontinuation if risks outweigh benefits.
- Safety checklist for patients:Start with low doses and increase slowly while tracking symptoms.Avoid mixing cannabis with alcohol or benzodiazepines unless advised by your clinician.Keep your mental health team informed and schedule regular follow-ups.
Following these steps reduces risk and supports safer, evidence-informed use for anxiety and PTSD.
Where Can You Find a Qualified Medical Marijuana Doctor in Naples?
Finding a qualified doctor in Naples starts with verifying that the clinician is authorized to certify patients in Florida’s medical marijuana registry and that they have experience treating mental health conditions with a measured, evidence-based approach. Look for clinicians who use standardized assessment tools, coordinate with psychiatry and psychotherapy, and provide clear follow-up and outcome measurement plans; these attributes indicate a safer, more integrated care model. Patients can prepare for selection conversations by asking about the clinician’s approach to product selection, dosing strategy, monitoring, and how they handle potential drug interactions or adverse events. Transparent clinicians will discuss alternatives and set realistic expectations rather than promising cures, helping patients make informed choices.
How to Choose the Right Medical Marijuana Doctor for Anxiety and PTSD?
Choosing the right clinician involves asking targeted questions about experience with anxiety and PTSD, approach to dosing and product selection, coordination with mental health providers, and follow-up procedures to monitor outcomes and side effects. Seek clinicians who use validated screening tools, emphasize conservative THC exposure, and require documentation of prior treatments when indicated, since these practices promote safer, evidence-aligned care. Avoid providers who guarantee cures or recommend high-THC regimens as first-line therapy; instead, prioritize those who integrate cannabis as one component of a comprehensive treatment plan. A structured onboarding process and clear outcome metrics are signs of reputable clinical practice.
- Questions to ask prospective clinicians:How do you assess suitability for medical cannabis in anxiety/PTSD?What product profiles and dosing strategies do you commonly recommend?How will you coordinate care with my mental health providers?
What Are the Costs and Insurance Considerations in Naples?
Costs for medical cannabis care typically include the clinician evaluation and the ongoing cost of cannabis products, and coverage by health insurance is generally limited for medical cannabis in the current regulatory landscape. Patients often encounter an out-of-pocket fee for the initial certification visit and for subsequent follow-ups, and they bear the cost of dispensary purchases, which vary by product type and potency; budgeting for ongoing therapy is important. Some patients explore cost-saving options such as lower-dose regimens, product programs offered by dispensaries, or bulk purchasing strategies, but insurance support is rarely available. Discuss anticipated costs with a prospective clinician and plan for regular follow-up visits to optimize dosing and cost-effectiveness.
- Initial evaluation and follow-up: Expect separate fees for certification visits and periodic checks.
- Product costs: Vary by formulation, potency, and dispensary pricing; patients pay out-of-pocket.
- Insurance: Most insurers do not cover medical cannabis; verify with your plan and clinician.
Understanding these financial aspects helps patients in Naples plan care responsibly and weigh the cost-benefit of cannabis as part of a broader treatment strategy.